Introduction
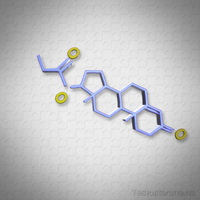
Hypogonadism, characterized by the body's inability to produce sufficient testosterone, has been increasingly recognized as a significant health concern among American males. This condition not only impacts sexual health but also has broader implications on overall well-being, including muscle mass, bone density, and mood regulation. The prevalence of hypogonadism is particularly noteworthy among individuals living with HIV, where the interplay between hormonal and immunological factors may exacerbate the condition. This article delves into a cross-sectional study that explores the prevalence of hypogonadism in American males with HIV, shedding light on the critical hormonal and immunological markers associated with this condition.
Study Design and Methodology
The study in question adopted a cross-sectional design to evaluate the prevalence of hypogonadism among a cohort of American males diagnosed with HIV. Participants were recruited from various HIV clinics across the United States, ensuring a diverse representation of socio-economic and ethnic backgrounds. Key hormonal markers, including total testosterone, free testosterone, and luteinizing hormone (LH), were measured to assess hypogonadal status. Additionally, immunological markers such as CD4 count and viral load were analyzed to understand their correlation with hypogonadism.
Prevalence of Hypogonadism in the HIV Population
The findings of the study revealed a significant prevalence of hypogonadism among American males with HIV, with approximately 30% of the participants exhibiting low testosterone levels. This rate is considerably higher than that observed in the general population, underscoring the heightened risk faced by individuals with HIV. The study also highlighted that hypogonadism was more prevalent among older participants and those with advanced stages of HIV, suggesting a possible link between disease progression and hormonal imbalance.
Hormonal Markers and Their Implications
The analysis of hormonal markers provided critical insights into the mechanisms underlying hypogonadism in the study population. Low levels of total and free testosterone were strongly associated with hypogonadism, while elevated levels of LH indicated primary hypogonadism in a subset of participants. These findings suggest that the hypogonadism observed in American males with HIV may be attributed to both testicular dysfunction and hypothalamic-pituitary axis disturbances, necessitating a multifaceted approach to treatment and management.
Immunological Markers and Their Correlation
The study also explored the relationship between hypogonadism and immunological markers, revealing a significant correlation between low testosterone levels and reduced CD4 counts. Participants with hypogonadism were more likely to have lower CD4 counts, indicating a compromised immune system. This association underscores the potential role of testosterone in immune function and suggests that hypogonadism may contribute to the progression of HIV by weakening the body's defense mechanisms.
Clinical Implications and Future Directions
The high prevalence of hypogonadism among American males with HIV necessitates increased awareness and screening efforts within the clinical community. Early detection and intervention can significantly improve the quality of life for affected individuals, mitigating the adverse effects of low testosterone on both physical and mental health. Future research should focus on longitudinal studies to better understand the temporal relationship between HIV progression and hypogonadism, as well as the efficacy of testosterone replacement therapy in this population.
Conclusion
This cross-sectional study provides compelling evidence of the elevated prevalence of hypogonadism among American males with HIV, highlighting the importance of hormonal and immunological markers in understanding this condition. The findings underscore the need for targeted screening and intervention strategies to address hypogonadism in this vulnerable population, ultimately enhancing the overall health and well-being of individuals living with HIV.
Contact Us For A Fast And Professional Response

- Unveiling the Link Between Hypogonadism and Mental Health: A Comprehensive Guide for American Males [Last Updated On: February 19th, 2025] [Originally Added On: February 19th, 2025]
- Unveiling the Best Practices in Medical Monitoring for Hypogonadism in American Males [Last Updated On: February 20th, 2025] [Originally Added On: February 20th, 2025]
- Hypogonadism and Sleep Disorders: A Bidirectional Link in American Males [Last Updated On: March 4th, 2025] [Originally Added On: March 4th, 2025]
- Unveiling the Link Between Hypogonadism and Muscle Health in American Males: A Medical Perspective [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Navigating Hypogonadism in Men with Autoimmune Diseases: A Comprehensive Guide [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Exploring the Link Between Hypogonadism and Impaired Wound Healing in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Exploring the Interplay Between Hypogonadism and Parathyroid Health in American Males [Last Updated On: March 16th, 2025] [Originally Added On: March 16th, 2025]
- Hypogonadism in American Males: Diagnosis, Testosterone Therapy, and Individualized Treatment Considerations [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Exploring Hypogonadism and Chronic Pain: Diagnosis, Treatment, and Holistic Management [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Hypogonadism in American Males: Diagnosis, Treatment, and Education Essentials for Physicians [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Hypogonadism and Prostate Health: Understanding, Managing, and Preventing Complications [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Hypogonadism and Thyroid Dysfunction: Exploring the Correlation in American Males [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- Hypogonadism and Autoimmune Disorders: Impact, Management, and Future Research in American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Hypogonadism and Liver Health: A Comprehensive Guide for American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Hypogonadism's Impact on American Men: Diagnosis, Treatment, and Quality of Life Enhancement [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Medical Imaging's Crucial Role in Diagnosing Hypogonadism in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Exercise as a Complementary Approach to Managing Hypogonadism in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Alternative Medicine Approaches for Managing Hypogonadism in American Males: A Review [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Managing Hypogonadism and Kidney Disease: Strategies for American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Ethical Challenges in Hypogonadism Treatment: Balancing Benefits, Risks, and Societal Pressures [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypogonadism's Impact on Bone Health: Diagnosis, Treatments, and Emerging Therapies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypogonadism and Hair Loss: Understanding Links and Exploring Treatments [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Hypogonadism's Impact on Respiratory Health in American Males: A Comprehensive Overview [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Advanced Medical Technologies Transform Hypogonadism Diagnosis in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Hypogonadism in American Males: Screening, Diagnosis, and Management Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Hypogonadism and Anemia: Diagnosis, Management, and Enhancing Men's Health Quality [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism's Neurological Risks: Cognitive Decline, Mood Disorders, and Neurodegenerative Diseases in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Monitoring Hypogonadism in Long-Term Care: Strategies and Technology for Enhanced Quality of Life [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Understanding Hypogonadism: Symptoms, Causes, and Comprehensive Management Strategies [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism's Impact on Skin Health and Testosterone Replacement Therapy Benefits [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism and Cancer Risk: Understanding the Link and Managing Health [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism's Impact on Muscle Health in American Males: Diagnosis, Treatment, and Research [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism and Allergies: Exploring Hormonal Links and Treatment Implications in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism and Hearing Loss: A Critical Connection in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Hypogonadism's Impact on Immune Function in American Males: Research and Clinical Insights [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism's Impact on Joint Health and Benefits of Testosterone Therapy [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism's Impact on Eye Health: Dry Eye, Cataracts, Glaucoma, and TRT Benefits [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism's Psychological Impact and the Crucial Role of Tailored Counseling [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism in American Males: Trends, Treatments, and Future Research Directions [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism and Headaches: Symptoms, Diagnosis, and Holistic Treatment Strategies [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Revolutionizing Hypogonadism Treatment: Innovations and Hope for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Hypogonadism's Impact on Gastrointestinal Health in American Males: A Comprehensive Analysis [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Medical Nutrition Therapy Enhances Hypogonadism Management in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Hypogonadism: Roles of Endocrinologists, Urologists, and Multidisciplinary Teams [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypogonadism's Impact on Dental Health: Symptoms, Management, and Holistic Care [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Preventing Hypogonadism: Strategies for At-Risk American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypogonadism in Transgender Men: Diagnosis, Treatment, and Personalized Care [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Medical Social Workers: Vital Support for American Males with Hypogonadism [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypogonadism's Emotional Impact on American Men: A Holistic Treatment Approach [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypogonadism's Impact on Blood Pressure: Causes, Links, and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypogonadism and Vision: Symptoms, Diagnosis, and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Hypogonadism's Impact on Cognitive Function in American Males: A Review and Outlook [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Managing Hypogonadism: Diagnosis, Treatment, and Lifestyle Strategies for American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Medical Rehabilitation for Hypogonadism: Enhancing Recovery in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Hypogonadism and Cholesterol: Implications for Cardiovascular Health in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- Hypogonadism's Impact on Balance: A Crucial Health Concern for American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Exploring the Link Between Hypogonadism and GERD in American Males: Diagnosis and Treatment [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Hypogonadism's Impact on Urinary Health: Diagnosis, Management, and Prevention Strategies [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Hypogonadism's Link to Peripheral Neuropathy: Insights and Treatment Options for Men [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Managing Hypogonadism-Related Fatigue: Therapies and Lifestyle Solutions for American Males [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Hypogonadism Linked to Accelerated Skin Aging: Insights and Interventions for American Males [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Strategies to Enhance Adherence to Hypogonadism Treatment in American Males [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Hypogonadism's Impact on Sinus Health in American Males: A Comprehensive Overview [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Hypogonadism and Gallbladder Health: Exploring the Link in American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Hypogonadism's Impact on Nail Health: Diagnosis, Treatment, and Lifestyle Management [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Medical Devices Revolutionize Hypogonadism Management in American Males [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Understanding Hypogonadism: Symptoms, Causes, and Treatment for American Males [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Hypogonadism Linked to Lymphatic Dysfunction in American Males: Study Insights [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Hypogonadism and Spleen Health: Exploring Links in American Males [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Hypogonadism's Impact on Ear Health: Symptoms, Diagnosis, and Management Strategies [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Understanding Hypogonadism: Nursing Roles in Diagnosis, Treatment, and Patient Care [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Managing Hypogonadism in American Males with Chronic Illnesses: Strategies and Insights [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- Hypogonadism's Impact on Wound Healing in American Males: Causes and Management Strategies [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Medical Counseling: Essential for Managing Hypogonadism in American Males [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Hypogonadism and Parathyroid Health: Impacts on American Male Bone Health and Well-being [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Hypogonadism's Impact on Thymus Health: Diagnosis, Management, and Future Research [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Hypogonadism and Pancreatic Health: Diagnosis and Integrated Care Strategies for American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Hypogonadism's Impact on Endocrine Balance in American Males: Symptoms, Effects, and Treatment [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Hypogonadism's Impact on Adrenal Function: Insights for American Males [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Hypogonadism and Autoimmune Diseases: Challenges and Management Strategies in American Males [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]