Introduction
Chronic pain is a pervasive health issue affecting millions of American men, with significant implications for their overall well-being and quality of life. Recent research has begun to explore the intricate relationship between chronic pain and hormonal regulation, particularly the impact on testosterone levels. This article delves into a longitudinal study that examines how chronic pain influences testosterone in American men, shedding light on the complex interplay between pain, hormones, and health.
Understanding Chronic Pain and Its Prevalence
Chronic pain, defined as pain lasting longer than three months, is a common condition among American men. According to the Centers for Disease Control and Prevention (CDC), approximately 20% of adults in the United States suffer from chronic pain, with a significant portion being male. The causes of chronic pain are diverse, ranging from musculoskeletal disorders to neuropathic conditions, and its impact extends beyond physical discomfort to affect mental health, sleep quality, and daily functioning.
The Role of Testosterone in Men's Health
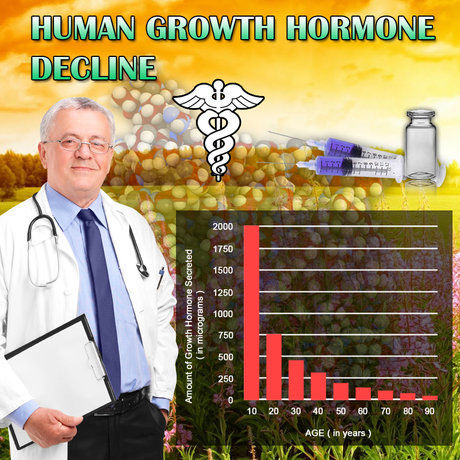
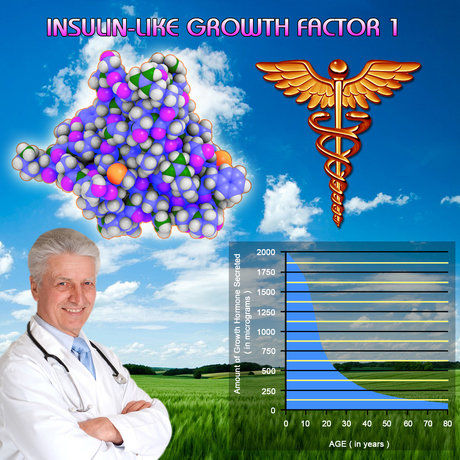
Testosterone is a crucial hormone in men, playing a vital role in regulating various bodily functions, including muscle mass, bone density, red blood cell production, and libido. Optimal testosterone levels are essential for maintaining physical and mental health. However, factors such as age, lifestyle, and underlying health conditions can influence testosterone production and regulation.
The Link Between Chronic Pain and Testosterone Levels
Recent studies have suggested a bidirectional relationship between chronic pain and testosterone levels. Chronic pain can lead to decreased testosterone production due to its impact on the hypothalamic-pituitary-gonadal (HPG) axis, which is responsible for regulating testosterone synthesis. Conversely, low testosterone levels may exacerbate pain sensitivity, creating a vicious cycle that can be challenging to break.
Longitudinal Study Insights
A longitudinal study conducted over five years followed a cohort of 500 American men aged 30 to 65, all of whom were diagnosed with chronic pain. The study aimed to assess the impact of chronic pain on testosterone levels and its implications for men's health. Participants underwent regular blood tests to measure testosterone levels, alongside assessments of pain intensity, quality of life, and mental health.
The findings revealed a significant correlation between chronic pain and reduced testosterone levels. Men with higher pain scores exhibited lower testosterone levels over time, with a notable decline observed in those with severe chronic pain. Additionally, the study found that men with low testosterone levels reported increased pain sensitivity and reduced pain tolerance, supporting the hypothesis of a bidirectional relationship.
Implications for Treatment and Management
The study's results highlight the importance of addressing both chronic pain and testosterone levels in the treatment and management of affected American men. Multimodal approaches that combine pain management strategies with hormone therapy may offer a more comprehensive solution. Pain management techniques such as physical therapy, cognitive-behavioral therapy, and pharmacological interventions can help alleviate symptoms and improve quality of life.
For men with low testosterone levels, hormone replacement therapy (HRT) may be considered, under the guidance of a healthcare professional. HRT can help restore testosterone levels to normal ranges, potentially reducing pain sensitivity and improving overall health outcomes. However, the decision to pursue HRT should be made on an individual basis, considering factors such as age, overall health, and potential side effects.
Conclusion
The longitudinal study on the impact of chronic pain on testosterone levels in American men underscores the complex relationship between pain and hormonal regulation. Chronic pain can significantly affect testosterone production, leading to a range of health issues that extend beyond physical discomfort. By understanding this relationship, healthcare providers can develop more effective treatment plans that address both pain and hormonal imbalances, ultimately improving the quality of life for affected men.
As research continues to unravel the intricacies of chronic pain and testosterone, it is crucial for American men to seek comprehensive care that considers all aspects of their health. Through a combination of pain management and hormone therapy, men can take proactive steps toward better health and well-being.
Contact Us For A Fast And Professional Response

- 0001) Genetics and Testosterone: American Males' Predisposition and Health Implications [Last Updated On: January 30th, 2026] [Originally Added On: February 19th, 2025]
- 0002) Fueling Masculinity: Unleashing the Power of Testosterone [Last Updated On: February 25th, 2025] [Originally Added On: February 25th, 2025]
- 0003) Decoding Testosterone: Unraveling the Impact of the Master Hormone on Your Existence [Last Updated On: February 26th, 2025] [Originally Added On: February 26th, 2025]
- 0004) The Evolving Chronicle of Testosterone: A Voyage Through Time [Last Updated On: February 27th, 2025] [Originally Added On: February 27th, 2025]
- 0005) The Unexplored Power: Advantages of Optimum Testosterone Levels beyond Muscle Development [Last Updated On: February 28th, 2025] [Originally Added On: February 28th, 2025]
- 0006) Decoding the Testosterone Code: Dissecting Myths and Misconceptions [Last Updated On: February 28th, 2025] [Originally Added On: February 28th, 2025]
- 0007) Unveiling the Vital Role of Testosterone in Women's Health: A Comprehensive Overview [Last Updated On: March 1st, 2025] [Originally Added On: March 1st, 2025]
- 0008) Unraveling the Powerhouse of Vitality: The Definitive Guide to Understanding Testosterone [Last Updated On: March 1st, 2025] [Originally Added On: March 1st, 2025]
- 0009) Unlocking Male Vitality: A Dietary Approach to Elevating Testosterone Levels Naturally [Last Updated On: March 2nd, 2025] [Originally Added On: March 2nd, 2025]
- 0010) Enhancing Testosterone Production through Physical Activity: The Impact of Resistance Training and HIIT on Hormonal Health [Last Updated On: March 3rd, 2025] [Originally Added On: March 3rd, 2025]
- 0011) Understanding Testosterone's Impact on Male Confidence and Mental Health [Last Updated On: March 4th, 2025] [Originally Added On: March 4th, 2025]
- 0012) Understanding Testosterone's Role in Male Health and Strategies to Maintain Its Levels [Last Updated On: March 5th, 2025] [Originally Added On: March 5th, 2025]
- 0013) Comprehensive Guide to Testosterone: Importance, Functions, and Lifecycle in Men [Last Updated On: March 6th, 2025] [Originally Added On: March 6th, 2025]
- 0014) Optimizing Men's Health: Boost Testosterone Naturally Through Diet, Exercise, and Lifestyle Changes [Last Updated On: March 7th, 2025] [Originally Added On: March 7th, 2025]
- 0015) The Evolution of Testosterone Therapy: Innovations, Safety, and Future Potential for Men's Health [Last Updated On: March 8th, 2025] [Originally Added On: March 8th, 2025]
- 0016) Managing Testosterone Decline in Aging Men: Strategies for Vitality and Quality of Life [Last Updated On: March 9th, 2025] [Originally Added On: March 9th, 2025]
- 0017) Maximizing Masculine Vitality: The Crucial Role of Sleep in Testosterone Regulation [Last Updated On: March 12th, 2025] [Originally Added On: March 12th, 2025]
- 0018) Exploring the Horizon: The Future of Hormonal Health and Testosterone Research Trends [Last Updated On: March 13th, 2025] [Originally Added On: March 13th, 2025]
- 0019) Unraveling the Nexus of Stress, Cortisol, and Testosterone: A Guide to Hormonal Equilibrium for American Men [Last Updated On: March 13th, 2025] [Originally Added On: March 13th, 2025]
- 0020) Unleashing Athletic Potential: The Role of Testosterone in Performance Enhancement [Last Updated On: March 15th, 2025] [Originally Added On: March 15th, 2025]
- 0021) Testosterone's Impact on Mood, Memory, and Motivation in American Males [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- 0022) Resistance Training Boosts Testosterone: A Guide for American Males [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- 0023) Testosterone's Impact on Bone Density in American Males: Mechanisms and Management [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- 0024) Testosterone's Crucial Role in Enhancing Immune Function in American Men [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- 0025) Testosterone Health for American Males: Supplements, Lifestyle, and Medical Options [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- 0026) Testosterone's Impact on Metabolism and Fat Burning in American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- 0027) Testosterone's Impact on Cardiovascular Health in American Men: Risks and Benefits [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- 0028) Hormonal Balance in Men: Testosterone, Estrogen, and Beyond for Optimal Health [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- 0029) Testosterone's Role in Enhancing Workplace Productivity and Drive in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- 0030) Environmental Toxins and Their Impact on Men's Testosterone Levels: A Comprehensive Overview [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0031) Testosterone's Role in Male Libido: Strategies to Boost Desire and Intimacy [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0032) Testosterone's Vital Role in American Males' Cardiovascular Health and Fitness [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0033) Low Testosterone in Men: Symptoms, Causes, and Effective Management Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0034) Modern American Diet's Impact on Testosterone Levels and Mitigation Strategies [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0035) Testosterone Revolution: Redefining Masculinity and Enhancing Men's Health in America [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0036) Testosterone's Role in Muscle Recovery and Growth for American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0037) Testosterone's Impact on Cognitive Performance in American Males: A Comprehensive Analysis [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0038) Optimizing Testosterone in American Men Through Positive Mental Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0039) Meditation Boosts Testosterone: A Holistic Approach for American Males' Health [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0040) Understanding Testosterone: Importance, Symptoms, and Managing Health Proactively [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0041) Testosterone's Role in Sleep Quality: Strategies for American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0042) Understanding Testosterone: Levels, Factors, and Health Impacts for American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0043) Key Vitamins and Minerals Boosting Testosterone in American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0044) Testosterone's Impact on Body Image and Self-Esteem in American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0045) Boosting Testosterone: Diet, Exercise, Sleep, and Stress Management for American Men [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0046) Testosterone's Impact on Mental Health in American Men: Depression, Anxiety, and Cognition [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0047) Testosterone's Role in Longevity: Insights for American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0048) Creativity Boosts Testosterone: Music and Art's Role in Men's Health [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0049) Testosterone and Chronic Diseases: Management Strategies for American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0050) Exploring Testosterone Replacement Therapy: Benefits, Risks, and Realities for American Males [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0051) Declining Testosterone Levels in American Males: Trends, Causes, and Health Strategies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0052) Urban vs. Rural Living: Impacts on Testosterone Levels in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0053) Andropause: Understanding Male Menopause and Testosterone's Role in American Men's Health [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0054) Testosterone's Impact on Ambition and Success in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0055) Outdoor Activities Boost Testosterone: A Natural Health Strategy for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0056) Optimizing Testosterone: The Synergy of Rest and Nutrition for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0057) Intermittent Fasting: Boosting Testosterone Levels in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0058) Testosterone's Impact on Mental Resilience in American Men: Strategies and Insights [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0059) Testosterone's Influence on Risk-Taking in American Males: Biological and Social Factors [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0060) Testosterone Research Journey: From Lab to Clinic, Enhancing American Males' Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0061) Digital Tools Revolutionize Testosterone Monitoring for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0062) Testosterone's Impact on Athletic Performance: Myths, Facts, and Future Research for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0063) Balancing Work and Health: Strategies for American Men to Maintain Testosterone Levels [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0064) Low Testosterone: Health Condition's Economic Impact on Society and Workforce [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0065) Hormonal Health and Testosterone: Vital Insights for American Men's Well-being [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0066) Social Interactions Impact Testosterone Levels in American Males: A Comprehensive Study [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0067) Boost Testosterone Naturally with Resistance Band Workouts for American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0068) Gut Health's Impact on Testosterone Levels in American Males: A Comprehensive Overview [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0069) Personalized Medicine Revolutionizes Testosterone Therapy for American Males [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- 0070) Revolutionizing Male Health: Advanced Technologies in Testosterone Optimization [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- 0071) Testosterone's Impact on Male Skin, Hair, and Aesthetic Health Management [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- 0072) Testosterone's Dual Impact on Immune Health in American Men: Suppression and Protection [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- 0073) Testosterone and Body Composition: Optimizing Health for American Males [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- 0074) Testosterone's Comprehensive Impact on Men's Sexual Health and Well-being [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- 0075) Alcohol and Smoking: Impacts on Testosterone Levels in American Males [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- 0076) Acupuncture's Role in Enhancing Testosterone Levels in American Men: A Comprehensive Overview [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- 0077) HIIT Boosts Testosterone: Optimal Fitness Strategy for American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- 0078) Mindful Living Boosts Testosterone: Meditation, Yoga, Sleep, Nutrition, and Exercise for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- 0079) Exploring Testosterone Boosters: Efficacy, Types, and Safe Usage for American Men [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- 0080) Testosterone's Role in Social Dominance and Evolutionary Biology for American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]