Introduction
Testosterone undecanoate, a long-acting injectable form of testosterone, has been increasingly utilized in the management of hypogonadism among American males. This study aims to explore the impact of testosterone undecanoate on reproductive health, specifically focusing on its effects on fertility and sexual function. Given the rising prevalence of hypogonadism and its associated symptoms, understanding the therapeutic implications of testosterone undecanoate is crucial for urological practice.
The Prevalence of Hypogonadism in American Males
Hypogonadism, characterized by low testosterone levels, affects a significant portion of the American male population. Studies indicate that approximately 2-6% of men suffer from this condition, with the prevalence increasing with age. Symptoms such as decreased libido, erectile dysfunction, and infertility can profoundly impact quality of life. Consequently, effective management strategies, including the use of testosterone undecanoate, are essential.
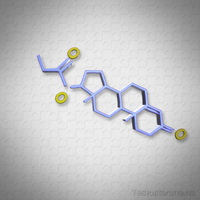
Mechanism of Action of Testosterone Undecanoate
Testosterone undecanoate is administered via intramuscular injection, providing a sustained release of testosterone over several weeks. This formulation maintains stable serum testosterone levels, mimicking the natural circadian rhythm of testosterone secretion. By doing so, it addresses the hormonal deficiencies associated with hypogonadism, thereby potentially improving reproductive health outcomes.
Impact on Fertility
One of the primary concerns regarding testosterone therapy is its potential impact on fertility. Testosterone undecanoate can suppress the hypothalamic-pituitary-gonadal axis, leading to reduced sperm production. However, recent studies suggest that this suppression may be reversible upon cessation of therapy. Moreover, some patients may benefit from adjunctive therapies, such as human chorionic gonadotropin (hCG), to maintain fertility while undergoing testosterone treatment. Thus, careful monitoring and individualized treatment plans are crucial for men wishing to preserve their reproductive potential.
Effects on Sexual Function
Testosterone undecanoate has shown promising results in improving sexual function among hypogonadal men. Clinical trials have demonstrated significant enhancements in libido, erectile function, and overall sexual satisfaction. These improvements are likely due to the restoration of normal testosterone levels, which play a critical role in sexual desire and performance. Therefore, testosterone undecanoate can be a valuable tool in the management of sexual dysfunction associated with hypogonadism.
Safety and Side Effects
While testosterone undecanoate is generally well-tolerated, it is not without potential side effects. Common adverse reactions include acne, increased hematocrit, and mood swings. More serious concerns, such as cardiovascular risks, have been debated in the literature. However, recent meta-analyses suggest that, when used appropriately, testosterone therapy does not significantly increase the risk of cardiovascular events. Nonetheless, regular monitoring of hematocrit, prostate health, and cardiovascular risk factors is recommended to ensure patient safety.
Clinical Considerations and Future Directions
In clinical practice, the decision to initiate testosterone undecanoate therapy should be based on a thorough evaluation of the patient's symptoms, testosterone levels, and reproductive goals. It is imperative to engage in shared decision-making, discussing the potential benefits and risks with the patient. Future research should focus on optimizing dosing regimens, exploring adjunctive therapies to preserve fertility, and further elucidating the long-term safety profile of testosterone undecanoate.
Conclusion
Testosterone undecanoate represents a significant advancement in the management of hypogonadism among American males. Its ability to improve sexual function and potentially preserve fertility underscores its importance in urological care. By understanding its mechanisms and clinical implications, healthcare providers can better tailor treatment plans to meet the individual needs of their patients, ultimately enhancing reproductive health outcomes.
References
1. Bhasin, S., et al. "Testosterone Therapy in Men with Hypogonadism: An Endocrine Society Clinical Practice Guideline." The Journal of Clinical Endocrinology & Metabolism, vol. 103, no. 5, 2018, pp. 1715-1744.
2. Snyder, P.J., et al. "Effects of Testosterone Treatment in Older Men." The New England Journal of Medicine, vol. 374, no. 7, 2016, pp. 611-624.
3. Corona, G., et al. "Testosterone Supplementation and Sexual Function: A Meta-Analysis Study." The Journal of Sexual Medicine, vol. 11, no. 6, 2014, pp. 1577-1592.
Contact Us For A Fast And Professional Response

- 0001) Testosterone Undecanoate: Enhancing Athletic Performance in American Males - Benefits and Risks [Last Updated On: February 16th, 2026] [Originally Added On: February 21st, 2025]
- 0002) Testosterone Undecanoate: Long-Acting Treatment for Hypogonadism in American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- 0003) Maximizing Testosterone Undecanoate Benefits: Diet, Exercise, and Lifestyle for American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- 0004) Testosterone Undecanoate: Cultural Perceptions, Health Impacts, and Therapeutic Use in American Males [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- 0005) Testosterone Undecanoate: Long-Acting TRT for American Males with Hypogonadism [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- 0006) Safety and Efficacy of Testosterone Undecanoate for American Men: A Comprehensive Review [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- 0007) Testosterone Undecanoate Therapy: Importance of Regular Monitoring for American Men's Health [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- 0008) Testosterone Undecanoate: Enhancing Life Quality in American Men with Hypogonadism [Last Updated On: March 19th, 2025] [Originally Added On: March 19th, 2025]
- 0009) Testosterone Undecanoate: A Potential Aid in Weight Management for American Men [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- 0010) Testosterone Undecanoate: Combating Muscle Loss in Aging American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- 0011) Testosterone Undecanoate's Impact on Sleep Quality in American Males: Benefits and Risks [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- 0012) Testosterone Undecanoate's Impact on Skin Health in American Males: Benefits and Risks [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- 0013) Testosterone Undecanoate: Treating Hypogonadism and Dispelling Myths in Men's Health [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- 0014) Testosterone Undecanoate: A Promising Therapy for Chronic Fatigue in American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- 0015) Testosterone Undecanoate: A Breakthrough in Managing Andropause for American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0016) Testosterone Undecanoate's Dual Impact on Hair Growth in American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- 0017) Testosterone Undecanoate: A Long-Acting Solution for Sexual Dysfunction in Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0018) Testosterone Undecanoate: Enhancing Emotional Well-being in American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0019) Testosterone Undecanoate's Impact on Immune Function in American Men: Recent Findings [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0020) Testosterone Undecanoate: A Promising Adjunct for Diabetes Management in American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0021) Testosterone Undecanoate: Enhancing Longevity and Health in American Males [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- 0022) Testosterone Undecanoate's Impact on Digestive Health in American Males: A Comprehensive Analysis [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0023) Testosterone Undecanoate: Enhancing Endurance in American Men Through Hormone Therapy [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0024) Testosterone Undecanoate's Impact on Metabolic Health in American Men: Benefits and Risks [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0025) Tailoring Testosterone Undecanoate Therapy for Diverse American Male Populations [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0026) Testosterone Undecanoate: A Vital Therapy for Hypogonadism in American Male Veterans [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0027) Testosterone Undecanoate's Impact on Blood Pressure in American Men: A Comprehensive Review [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- 0028) Testosterone Undecanoate: Enhancing Fertility in American Men with Hypogonadism [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0029) Testosterone Undecanoate Enhances Cognitive Function in American Men: A Review [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0030) Economic Impact of Long-Acting Testosterone Undecanoate on U.S. Healthcare Costs [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0031) Testosterone Undecanoate: Enhancing Male Health in American Clinical Trials [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- 0032) Testosterone Undecanoate's Impact on Dental Health in American Males: Benefits and Risks [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0033) Testosterone Undecanoate: Enhancing Life Quality in American Male Cancer Survivors [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0034) Testosterone Undecanoate's Impact on Joint Health in American Men: Benefits and Risks [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0035) Testosterone Undecanoate: A Novel Approach to Managing Allergies in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0036) Testosterone Undecanoate's Impact on Liver Health in American Males: A Review [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0037) Testosterone Undecanoate: Enhancing Injury Recovery in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- 0038) Testosterone Undecanoate's Impact on Respiratory Health in American Men: Asthma and COPD [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0039) Testosterone Undecanoate: A Promising Therapy for Chronic Pain in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0040) Testosterone Undecanoate: Managing Side Effects in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0041) Testosterone Undecanoate: Enhancing Eye Health in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0042) Testosterone Undecanoate: Benefits and Management for American Men with Hypogonadism [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- 0043) Testosterone Undecanoate's Impact on Hearing in American Males: A New Research Insight [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0044) Testosterone Undecanoate: A Promising Treatment for Osteoporosis in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0045) Testosterone Undecanoate's Impact on Cholesterol Levels in American Men: A Comprehensive Review [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0046) Testosterone Undecanoate: A Promising Solution for Stress Management in American Males [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0047) Testosterone Undecanoate's Impact on Kidney Function in American Men: A Comprehensive Review [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0048) Testosterone Undecanoate: Enhancing Cognitive Performance in American Men [Last Updated On: March 28th, 2025] [Originally Added On: March 28th, 2025]
- 0049) Testosterone Undecanoate: Enhancing Reproductive Health in American Males [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- 0050) Testosterone Undecanoate Enhances Skin Elasticity in American Men with Hypogonadism [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- 0051) Testosterone Undecanoate: Dosage Adjustments for American Men with Hypogonadism [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- 0052) Testosterone Undecanoate and Hair Loss: Risks and Mitigation Strategies for American Men [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- 0053) Testosterone Undecanoate Enhances Nail Health in American Males with Hypogonadism [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- 0054) Testosterone Undecanoate Therapy: Monitoring, Optimization, and Long-Term Health for American Men [Last Updated On: March 31st, 2025] [Originally Added On: March 31st, 2025]
- 0055) Testosterone Undecanoate Boosts Immune Function in American Men: Clinical Insights [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- 0056) Testosterone Undecanoate: Enhancing Body Composition in American Males [Last Updated On: April 2nd, 2025] [Originally Added On: April 2nd, 2025]
- 0057) Testosterone Undecanoate: Enhancing Muscle Recovery in American Men [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- 0058) Testosterone Undecanoate: Thrombotic Risks and Monitoring in American Men [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- 0059) Testosterone Undecanoate's Impact on Glycemic Control in American Men with Hypogonadism [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- 0060) Testosterone Undecanoate: A Novel Approach to Managing Anxiety in American Males [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- 0061) Testosterone Undecanoate Enhances Bone Healing in American Men: A Comprehensive Review [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- 0062) Testosterone Undecanoate: Enhancing Muscle Strength in American Men [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- 0063) Testosterone Undecanoate: A Promising Treatment for Depression in American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- 0064) Testosterone Undecanoate: Skin Pigmentation Changes in American Males [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- 0065) Testosterone Undecanoate's Impact on Heart Rate in American Men: A Comprehensive Review [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- 0066) Testosterone Undecanoate: Enhancing Sexual Health in American Males with Hypogonadism [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- 0067) Managing Side Effects of Testosterone Undecanoate Therapy in American Men [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- 0068) Testosterone Undecanoate's Impact on Thermoregulation in American Men: Clinical Insights [Last Updated On: April 12th, 2025] [Originally Added On: April 12th, 2025]
- 0069) Testosterone Undecanoate's Impact on Appetite in American Males: A Comprehensive Review [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- 0070) Testosterone Undecanoate's Impact on Sleep Quality in American Men with Hypogonadism [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- 0071) Testosterone Undecanoate's Impact on Skin Hydration in American Males: A Comprehensive Review [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- 0072) Testosterone Undecanoate's Impact on Blood Viscosity in American Men: Monitoring and Management [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- 0073) Testosterone Undecanoate's Impact on Blood Flow in American Men: Benefits and Risks [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- 0074) Testosterone Undecanoate: Enhancing Male Aesthetics and Health in American Men [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- 0075) Testosterone Undecanoate: Enhancing Wound Healing in American Men [Last Updated On: April 18th, 2025] [Originally Added On: April 18th, 2025]
- 0076) Testosterone Undecanoate: A New Hope for Migraine Management in American Males [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- 0077) Testosterone Undecanoate: Enhancing TRT with Lifestyle Adjustments for American Men [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- 0078) Testosterone Undecanoate's Impact on Skin Sensitivity in American Males: Dermatological Insights [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- 0079) Testosterone Undecanoate Therapy: Benefits and Risks for American Males [Last Updated On: April 21st, 2025] [Originally Added On: April 21st, 2025]
- 0080) Testosterone Undecanoate's Impact on Skin Texture in American Males: Benefits and Challenges [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]